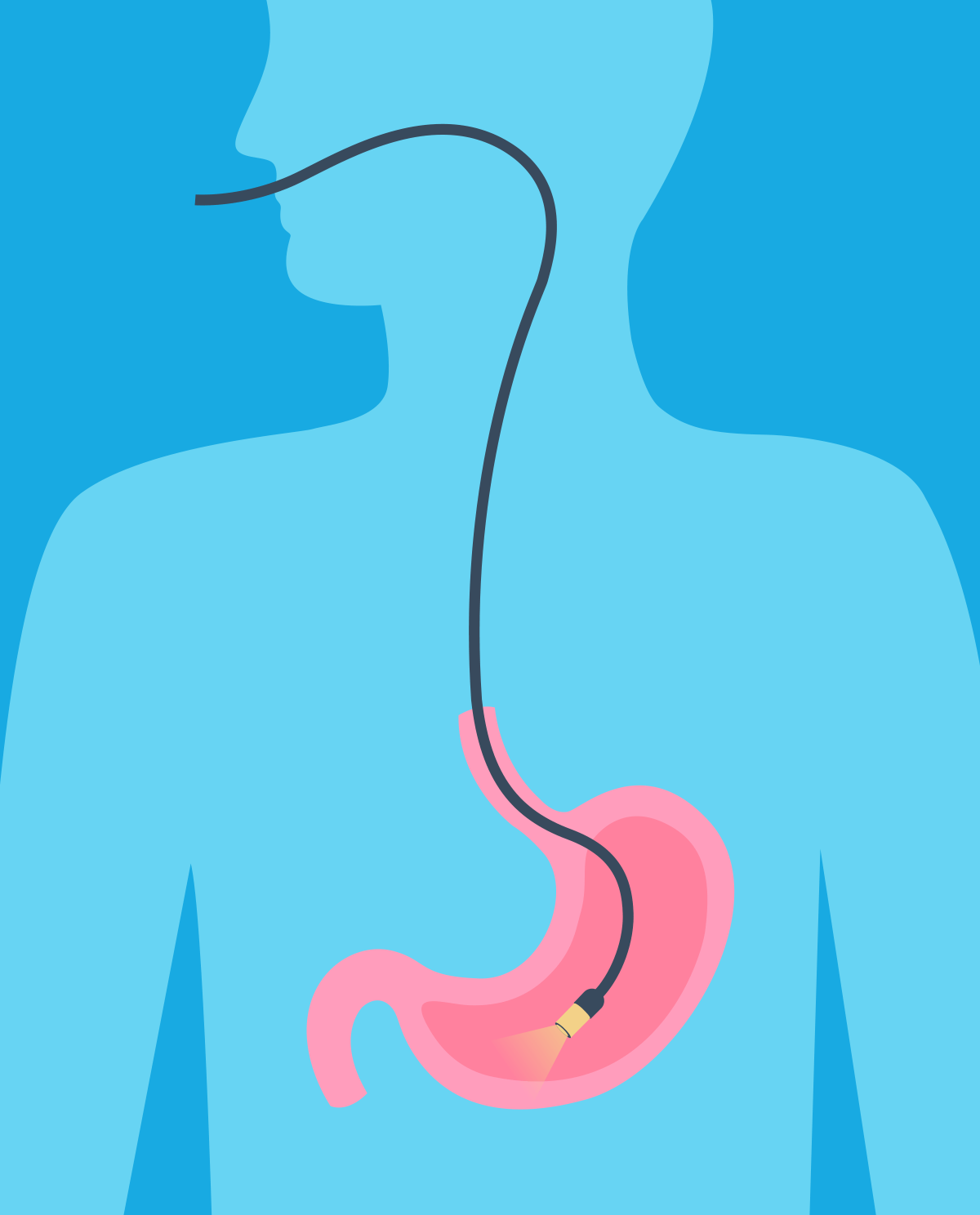
What happens during a gastroscopy?
A gastroscopy procedure lasts from a few to several minutes, during which time the patient assumes a position lying on the left side. Most often, the procedure is performed under local anesthesia of the throat with lidocaine spray, then a mouthpiece is put in, which prevents a patient from closing their mouth if discomfort is felt. Then, the doctor introduces a gastroscope into the mouth - a thin tube equipped with a light source and a camera, so that the doctor can examine the recorded image on the screen during the examination. Later in the procedure, the endoscope is inserted into the esophagus, stomach and duodenum (the first section of the small intestine).
Is a gastroscopy painful?
The examination itself is not painful but the moment when the device enters the esophagus can be unpleasant. In addition to this, retching and belching may occur. The patient may also experience discomfort associated with endoscope movements. It is possible to perform the procedure under sedation or general anesthesia, an anesthesiologist would be required for this form of anesthesia.
Indications for gastroscopy:
- epigastric complaints or pain felt below the ribs in the area of the upper abdomen (especially in combination with other symptoms suggestive of a serious illness, including cancer, or occurrence in patients over 45 years of age)
- collection of specimens or other material for histopathological or microbiological examination operations
- achalasia and symptomatic gastroesophageal reflux disease
- chronic vomiting of an unknown cause
- assessment of esophageal varices in a patient with portal hypertension and their ligation or sclerotherapy (method of treatment of varicose veins, which involves applying a chemical agent to the lumen of the vein, initiating a cycle of morphological changes in the walls of the varicose vein used to grow its lumen)
- iron deficiency anemia, when the location of pathologies in the load compartment is suspected.
- dysphagia (swallowing disorder) or odynophagia (pain on swallowing)
- suspected active bleeding or previous bleeding from the upper digestive tract
- further histopathological diagnosis of lesions found in other tests (e.g. thickening of the stomach wall used in ultrasound or computed tomography)
- familial adenomatous polyposis and familial colorectal cancer not associated with polyposis (HNPCC)
- assessment of a degree similar to chemical burns in the esophagus
- treatment of upper gastrointestinal bleeding
- removal of foreign bodies from the esophagus
- introduction of a tube (nutritional, decongestant) and production of nutritional fistulas (gastrostomy, jejunostomy)
- widening narrowed cancer and non-cancer nutritional meals
- excision of polypoid lesions
- treatment of early gastric cancer
- palliative treatment of esophageal and gastric cancer (ablation, implantation of self-expanding prostheses)
- endoscopic therapy of intestinal metaplasia
- treatment of postoperative complications in the upper anterior segment (stenosis, leak syndromes)
- oncological supervision and a patient with precancerous conditions (in patients with Barrett's esophagus, checks every 3 years, patients with HNPCC every 2 years over 30 years of age)
Contraindications to gastroscopy:
Absolute
- informed refusal to consent to an examination expressed by the patient
Relative
- acute coronary syndromes
- acute respiratory failure
- acute or chronic severe heart failure
- signs of acute surgical abdominal disease requiring surgery
- lack of cooperation during the examination
How can you prepare for a gastroscopy?
Do not eat anything 6-8 hours before a gastroscopy procedure, the last drink can be taken 4 hours before the procedure, in addition, do not smoke cigarettes or chew gum before this test. In preparation for a gastroscopy, a patient should remove movable prostheses, piercings, etc. from the mouth. After the procedure, it is not recommended for a patient to eat or drink anything for another 2 hours (risk of aspiration due to local anesthesia). People with illnesses that require regular medication (e.g. hypertension, heart disease, epilepsy and others) should take the morning dose of the drug with a small amount of water on the day of the study. Patients who use drugs that reduce blood clotting should consult a doctor before the examination to assess the need for discontinuation or substitution.
Complications after a gastroscopy
Gastroscopy as a method of invasive diagnostics is at risk of complications, both during and after its completion. The most common are complications associated with anesthesia (i.e. puncture hematoma, phlebitis, occurrence of adverse drug reactions, e.g. respiratory depression, hypotension, tachycardia, arrhythmias). In addition, there is a risk of the transmission of an infection through insufficiently disinfected equipment (mainly hepatitis B and C). Another complication may be mucosal damage or even gastrointestinal perforation, but this is extremely rare. After the examination, the patient may have a sore throat.
ATTENTION!
If any of the following occur soon after a gastroscopy
- fever
- severe stomach pain
- severe vomiting (especially if it includes blood or any appearance similar to coffee grounds)
- black, tarry stool
you should contact your doctor immediately.
This article was translated from Polish to English, the references below are those used in the Polish article.
- Interna Szczeklika 2018 Podręcznik Chorób Wewnętrznych, Autorzy: Piotr Gajewski, Andrzej Szczeklik Wydawnictwo: Medycyna Praktyczna
- https://www.mp.pl/pacjent/gastrologia/diagnostyka/51054,gastroskopia
- https://www.mp.pl/medycynarodzinna/artykuly/195669,endoskopia-gornego-odcinka-przewodu-pokarmowego-2018
- https://www.mp.pl/interna/chapter/B16.V.26.2.1