Why clarity matters in online medical consultations
In an in-person visit, a doctor can ask follow-up questions, examine you, and fill in gaps quickly. Online, your message is the starting point and (sometimes) the main source of information.
When a question is vague or disorganized, the clinician has to spend time reconstructing basics:
- what is happening (the observable facts),
- how it started and changed (the timeline),
- what context matters (history, meds, tests),
- what you want to know (the decision you are trying to make).
If those pieces are missing, the safest response often becomes general reassurance or a list of possibilities rather than clear next steps. Clear communication reduces misunderstandings, shortens back-and-forth, and increases the chance of receiving guidance that fits your situation.
Online medical consultations work best when doctors can quickly grasp the context, spot potential red flags, and understand what the patient is actually trying to figure out.
What information doctors need to help you effectively
More words do not equal more clarity. What helps most is relevant detail, in a predictable order.
A practical way to think about it:
- observations first (symptoms and facts),
- timeline second (how it evolved),
- context third (history, medications, tests),
- question last (what you are asking the doctor to interpret).
This order makes online consultation messages easier to scan and reduces the need for guesswork.
Symptoms: what, where, and since when
Describe symptoms as specifically as possible:
- what you are experiencing (in plain terms),
- where the symptoms occur (location or body area),
- when they started and how they have changed over time.
A few details that usually make a big difference:
- pattern: constant vs comes and goes; time of day; triggers; anything that reliably makes it better/worse,
- associated symptoms: what else appears alongside it (and what does not),
- what you have already tried: rest, hydration, over-the-counter meds, home measures, and whether they helped,
- impact: what it affects (sleep, appetite, work, exercise), without turning it into a long story.
Duration and progression often provide more insight than symptom intensity alone.
Timeline is more important than severity
Severity is subjective and can be hard to compare between patients. Time and change are easier to interpret clinically, especially in telemedicine where the doctor can’t examine you.
A short timeline helps a doctor understand the course:
- start: when it first appeared (approximate is fine),
- progression: improving, worsening, unchanged, or fluctuating,
- turning points: anything that changed the picture (new symptom, new medication, travel, illness exposure, stress, injury),
- current status: what it is like today.
Even a simple, compact line can improve the quality of the response:
"Started 10 days ago, worse on days 3–5, then improved; now stable but not fully gone."
Medical history and medications
Relevant medical history, chronic conditions, and current medications help doctors interpret symptoms and avoid unsafe assumptions. Even details that feel unrelated can matter in an online medical consultation.
Include what is most likely to change interpretation or safety:
- chronic diagnoses (if any),
- current prescription medications and doses (if you know them),
- supplements and over-the-counter meds you are actively using,
- recent medication changes (started/stopped/dose change),
- known allergies or prior reactions (especially to medications),
- relevant prior events (recent infections, procedures, hospitalizations, or similar episodes).
If you have test results, include the key facts (what test, when, and what it showed) rather than a conclusion. If possible, copy the numbers or the exact wording from the report.
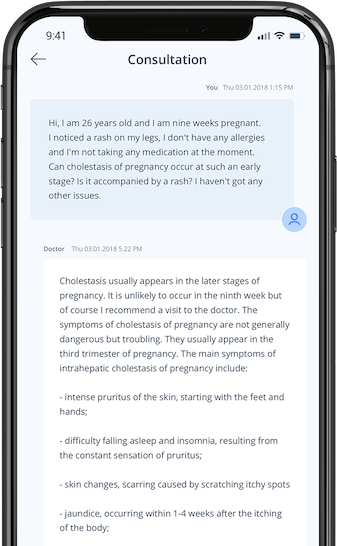
Examples: unclear vs well-written medical questions
An unclear question may describe symptoms without context, omit timelines, or focus on conclusions rather than observations. It often forces the doctor to guess what matters most.
Example (unclear):
"I feel weird and tired. Could this be something serious?"
What is missing:
- what "weird" means in concrete terms,
- how long it has been happening,
- whether it is changing,
- any relevant background,
- what you want the doctor to help decide.
A well-written question presents facts in a neutral, structured way, allowing the doctor to assess the situation without assumptions.
Example (well-written):
"Age/sex: 34M.
Main symptom: fatigue and low energy.
Timeline: started ~3 weeks ago, gradually worsening, no clear trigger.
Associated symptoms: mild headaches 2–3x/week; no fever.
Context: no chronic conditions, not on prescription meds; started an iron supplement 1 week ago, no change.
Question: what are the most likely causes to consider, and what information or tests would help narrow this down in an online consult?"
Another pair, showing the value of a timeline:
Example (unclear):
"I have stomach pain. What is it?"
Example (well-written):
"Age/sex: 28F.
Symptom: abdominal pain around the upper middle area.
Timeline: began yesterday evening, comes in waves, lasts 10–15 minutes, then eases.
Triggers: seems worse after eating; better when sitting still.
Associated symptoms: nausea, no vomiting.
Meds: ibuprofen taken once, no clear improvement.
History: no known GI conditions. Question: based on this pattern, what should I watch for, and what details would help you differentiate common causes?"
Common mistakes when asking medical questions online
Some of the most frequent issues include:
- combining multiple unrelated problems in one message,
- skipping important background information,
- focusing on self-diagnosis instead of symptoms,
- leaving out recent test results or previous diagnoses,
- burying key details inside a long, unstructured narrative.
A few practical corrections:
- Keep one main problem per message when possible. If you have two issues, separate them clearly and state which one is the priority.
- Avoid jumping straight to a conclusion ("I think it’s X"). Lead with observations and let the doctor interpret them.
- Do not assume the doctor sees your history. Restate the key parts that matter for this question.
- If you mention tests, include the timing and the result details. "Normal bloodwork" is less useful than "CBC and CRP done 2 weeks ago, both within range."
Avoiding these mistakes improves both clarity and efficiency.
For a broader comparison between automated tools and clinical reasoning, see this article on symptom checkers versus asking a doctor.
A simple template you can follow
Using a consistent structure makes it easier for doctors to understand your situation, especially in online consultations where follow-up questions may take time. A basic framework can include:
- age and sex,
- main symptoms,
- symptom duration and progression,
- known medical conditions,
- medications or supplements,
- your primary concern or question.
You can copy-paste and fill in a template like this:
- Age/sex:
- Main symptom(s):
- Where it happens:
- Start date (approx):
- Timeline/progression (better/worse/same; any turning points):
- Associated symptoms (present/absent):
- What I tried so far (and effect):
- Relevant medical history:
- Current medications/supplements (incl. recent changes):
- Recent tests/diagnoses (what/when/result):
- My main question (what I want help deciding):
This approach helps ensure that important information is not missed.
If you are preparing information for a more complex case or follow-up, this guide on preparing medical data for a second opinion may also be useful.
When a written medical question is not enough
While online questions can be useful, they are not always sufficient. Written messages cannot replace a physical exam, immediate monitoring, or urgent evaluation when symptoms are rapidly worsening or hard to assess remotely.
Situations involving rapidly worsening symptoms, severe pain, or neurological changes may require in-person evaluation. Knowing the limits of written consultations is part of responsible health decision-making.