What is chondromalacia?
The explanation of this disease should begin with a description of the cartilage in the knee joint. This cartilage can handle enormous loads, up to 65 times the weight of a person. The thickness of the cartilage ranges from 3 to 5 mm, it is to ensure adequate cushioning, protection of the subchondral tissue and smooth movements in the joint. The nutritional function for this tissue is performed by synovial fluid, which is produced during movement.
Due to the lack of vascularization, articular cartilage has no regenerative capacity - all types of defects resulting from injuries, dislocations or other injuries can be easily leveled by the formation of fibrous cartilage by subchondral tissue, but it is much less resistant to compressive forces than permanently damaged hyaline cartilage.
The term chondromalacia refers to the softening and structural changes of the patella cartilage in young people, however, it is currently popularly used even for patients over 60 years of age.
Cartilage that is thinner, softer, delaminates, or has defects, carries loads much worse, absorbs - in other words - performs its function worse. The descriptions of this disease distinguish four levels of advancement described in the following table.
Scale of chondromalacia according to Outerbridge:
Deep Grades III and IV cannot heal, leading to degenerative changes.
| Degree | Description |
|---|---|
| I | fluffiness and softening |
| II | Superficial damage - cracks (gaps <1.25 mm) |
| III | deep damage - cracks reaching the subchondral bone without exposing it (gaps > 1.25 mm) |
| IV | visible visible defects of the subchondral bone |
* grade 0 would mean healthy cartilage.
There are two types of knee osteoarthritis:
- primary - may arise as a result of minor injuries and overloads, deepen spontaneously,
- secondary - the cause of their occurrence is known, it can be e.g. trauma or a history of illness (in the literature for example sterile osteonecrosis during steroid treatment is given).
Possible causes for chondromalacia
- long-term immobilization of the joint,
- patella injury,
- too much muscle tension in the knee joint,
- muscle weakness in the knee joint,
- patella dislocation or fracture,
- sports excessively straining the knee joint - running, skiing, etc.,
- flat feet,
- lateral patella support,
- valgus or deformity of the knees,
- recurrent dislocation or subluxation of the patella.
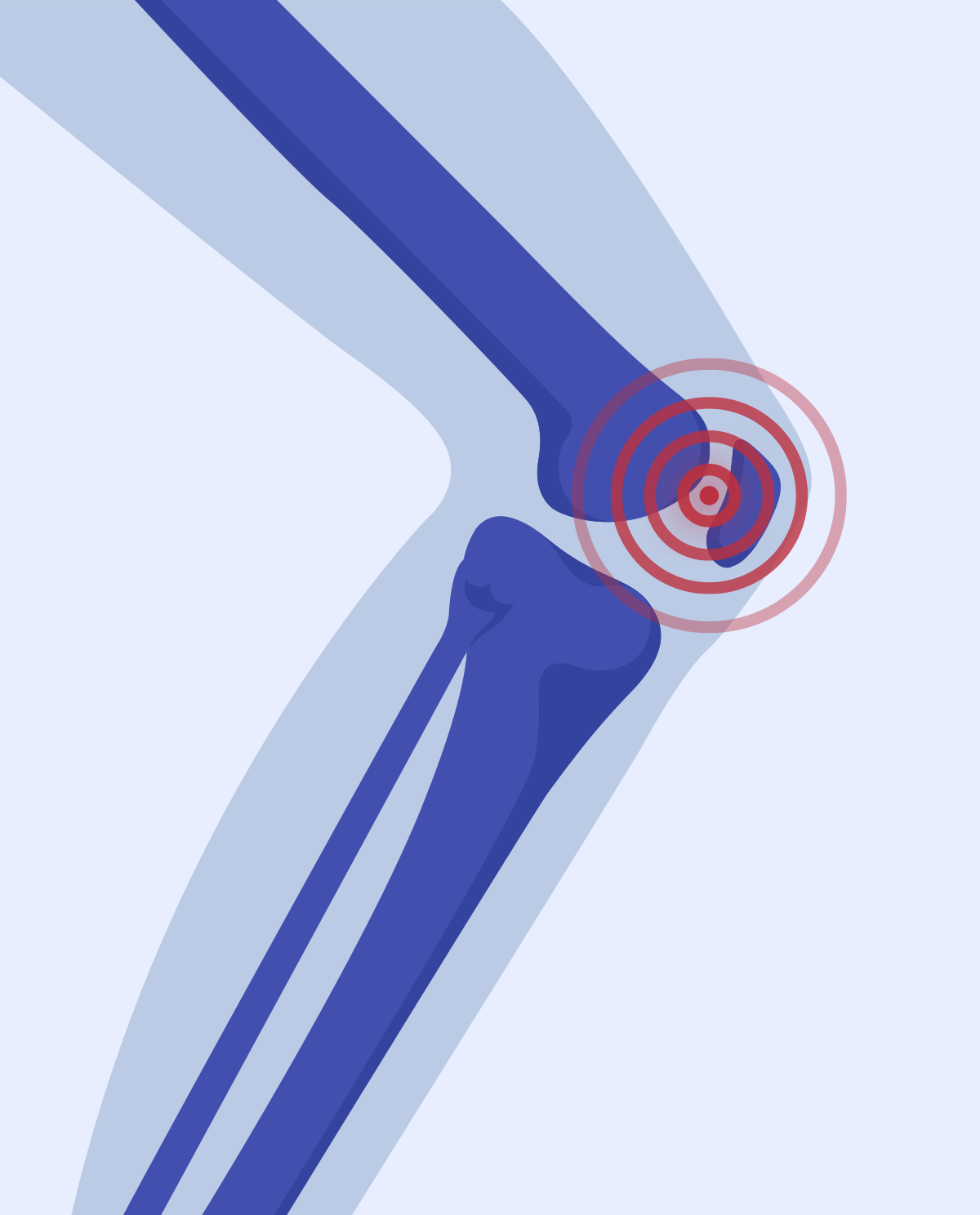
Knee pain
Appearing pain at the beginning of motor activity and after its termination, felt in the front part of the knee is one of the signals that may indicate chondromalacia. However, it is not confirmed experimentally or clinically why pain occurs despite the lack of cartilage innervation. In the case of softening, reduction of thickness and numerous defects, it is possible to transfer loads to the subchondral bone - but this has not been confirmed.
It also happens that the degree of chondromalacia is advanced and pain does not appear.
Available studies
Ultrasound, MRI or a classic X-ray are non-invasive tests that allow you to assess the state of cartilage in the joint. The best, but invasive way of introducing surgical instruments into the joint is arthroscopy.
Treatment
Chondromalacia patellae are treated primarily with movement, because it is usually caused by accumulating micro-injuries resulting from poor training (too high intensity or volume of training) in combination with poorly distributed load as a result of e.g. muscular imbalances. Joint cartilage is often compared to a dishwashing sponge: if you don't use it, it will dry out, it will crumble, but if you use it too often, you will damage it, so the biggest challenge in treating this condition is to find the 'golden mean’. Along with this comparison, it is logical that stillness is nothing but healing (it is symptomatic healing).
In the first phase of treatment, exercises to relax excessively tight muscles (usually the quadriceps muscle) are used, then strengthening exercises, stabilization exercises and characteristic movements of the sport discipline (when treating athletes) are implemented. In many cases, viscosupplementation, i.e. delivery of hyaluronic acid, is recommended.
See exercises for chondromalacia. In many cases, viscosupplementation, i.e. delivery of hyaluronic acid, is recommended.
In demanding cases, surgical treatment is used - the lesions are removed, the cartilage surface is cleaned, the cartilage surface is drilled (abrasion) or implants or transplants are performed.
How to prevent injuries - what shouldn’t you do?
Below are a few simple rules that can help you reduce the risk of injury.
- Take care of your weight - try to avoid being overweight.
- Watch out for the maximum range of motion (both bends and extensions).
- Make sure your workouts aren’t too intense.
- Strengthen weakened muscles.
- Don't run up or down the stairs.
- D. Witoński, Chondromalacia - recognition or nihilism diagnostic? Orthopedics Traumatologia Rehabilitacja MEDSPORTPRESS, 2016; 5 (6); Vol. 18, 508-510
- G. Adamczyk, Ł. Antolak, T. Skrok, R. Śmigielski, Early results of treatment of knee joint cartilage defects using autogenous cartilage and bone grafts by OATS method, Carolina Medical Center, Warsaw, Scientific consultant: prof. zw. dr hab. Artur Dziak
- https://www.youtube.com/channel/UCty9zs3xys93kx9USnlE7qg
- https://www.ortopedio.pl/porady-ekspertow/chondromalacja-rzepki-diagnostyka-kiedy-zdecydowac-sie-na-operacje/
- https://www.crse.org.pl/blog/137-jak-leczyc-chondromalacje-chrzastki-stawowej
- https://pl.wikipedia.org/wiki/Chondromalacja