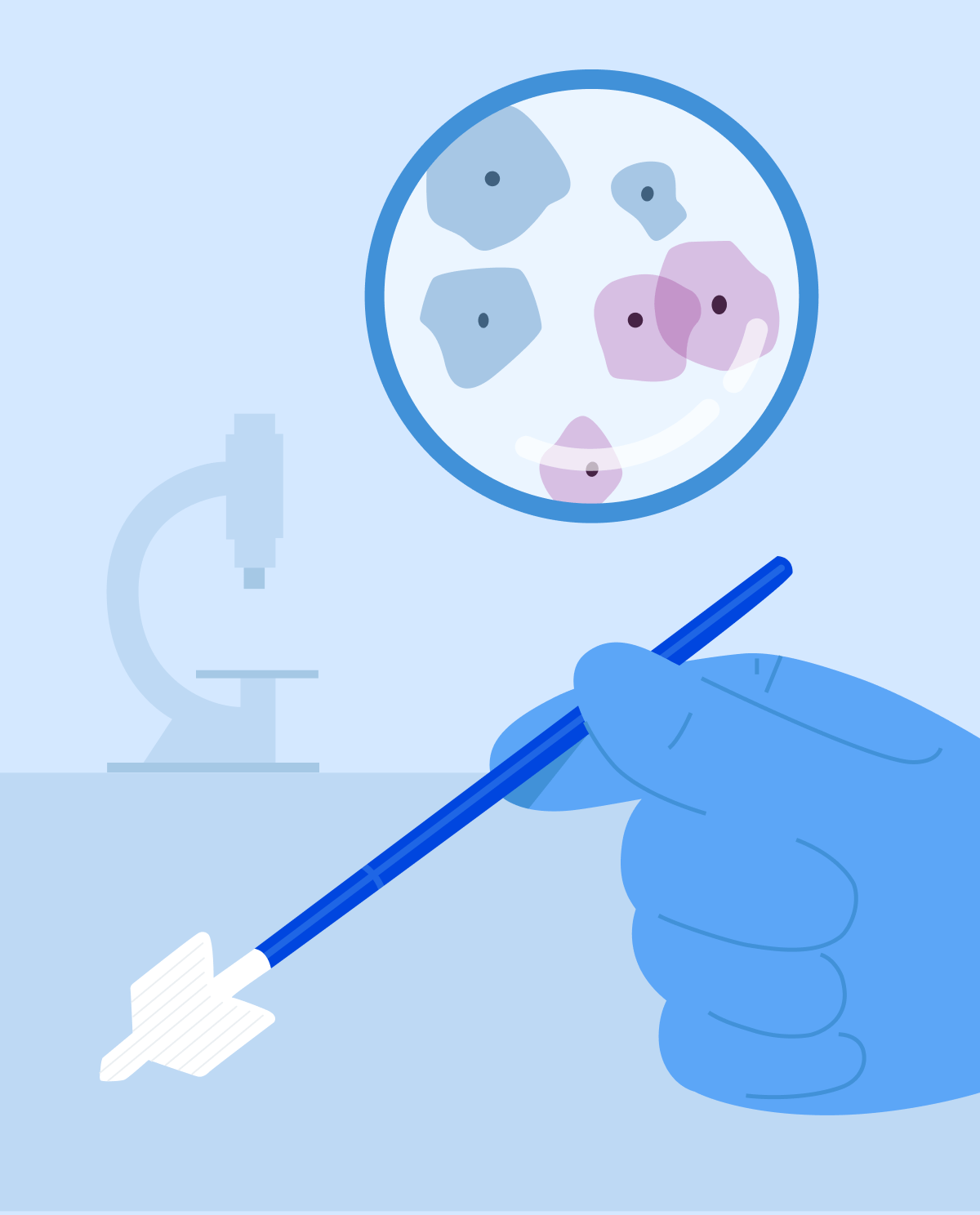
How these tests are performed
- Pap smear: your gynecologist will insert a speculum, which is a tube-shaped instrument to open the vagina. Using a soft brush, the physician will “brush” off cervical cells for inspection of abnormal/and/or cancer cells.
- Cervical screening is performed in the same manner, but the end result is to look for the presence of human papillomavirus (HPV).
How to prepare before the examination
- avoid intercourse,
- avoid douches,
- tampon use,
- any medication or anti-contraceptive gel/foam/cream or other intra-vaginal medication.
When and how often should they be performed
- Women between the ages of 21 and 29: if the pap test results are normal, your gynecologist will propose for you to get re-tested in 3 years. If the Pap/HPV co-test is available and normal, it is recommended to test again in 5 years.
- Women between the age of 30 to 65: same guidelines as women from 21 to 29 years of age.
- Women older than 65: shouldn’t be tested if a total hysterectomy has been done or if constant screening has been normal for several years.
What will be done in case of unwanted results
- Positive HPV but normal pap: this occurs in many women. The infection usually clears up within 2 years. Your gynecologist may refer you for a follow-up test within a year or two, if the infection is still present, you may need a colposcopy (your gynecologist will use a colposcope to better visualize your cervix, vulva, and vagina for abnormal tissue).
- Inflammatory process detected: this could mask invasive cancer thus the infection must be treated, and a pap follow-up must be performed within 3-6 months. If abnormality persists, you will be referred for a colposcopy.
- ASCUS (atypical squamous cells of undetermined significance) positive: this presents the most common abnormality noted in pap smears. It may signify an ongoing infection with HPV or yeast. A follow-up pap smear should be performed within 3-6 months but if abnormal cells persist, you will be referred for a colposcopy.
- LSIL (low-grade squamous intraepithelial lesion) and HSIL (high-grade squamous intraepithelial lesion): this depicts the presence of cancerous cells; your gynecologist will refer you for a colposcopy accompanied by biopsy
- Invasive cancer: biopsy if the growth of the tumor is evident or you will be referred for a colposcopy accompanied by biopsy.
- AGUS (abnormal glandular cells of undetermined significance): in this case, colposcopy and biopsy will be required and then followed by what we call a cone biopsy (to remove all abnormal cells) and dilation/curettage (a procedure that is both diagnostic and therapeutic to remove all residual abnormal cells).