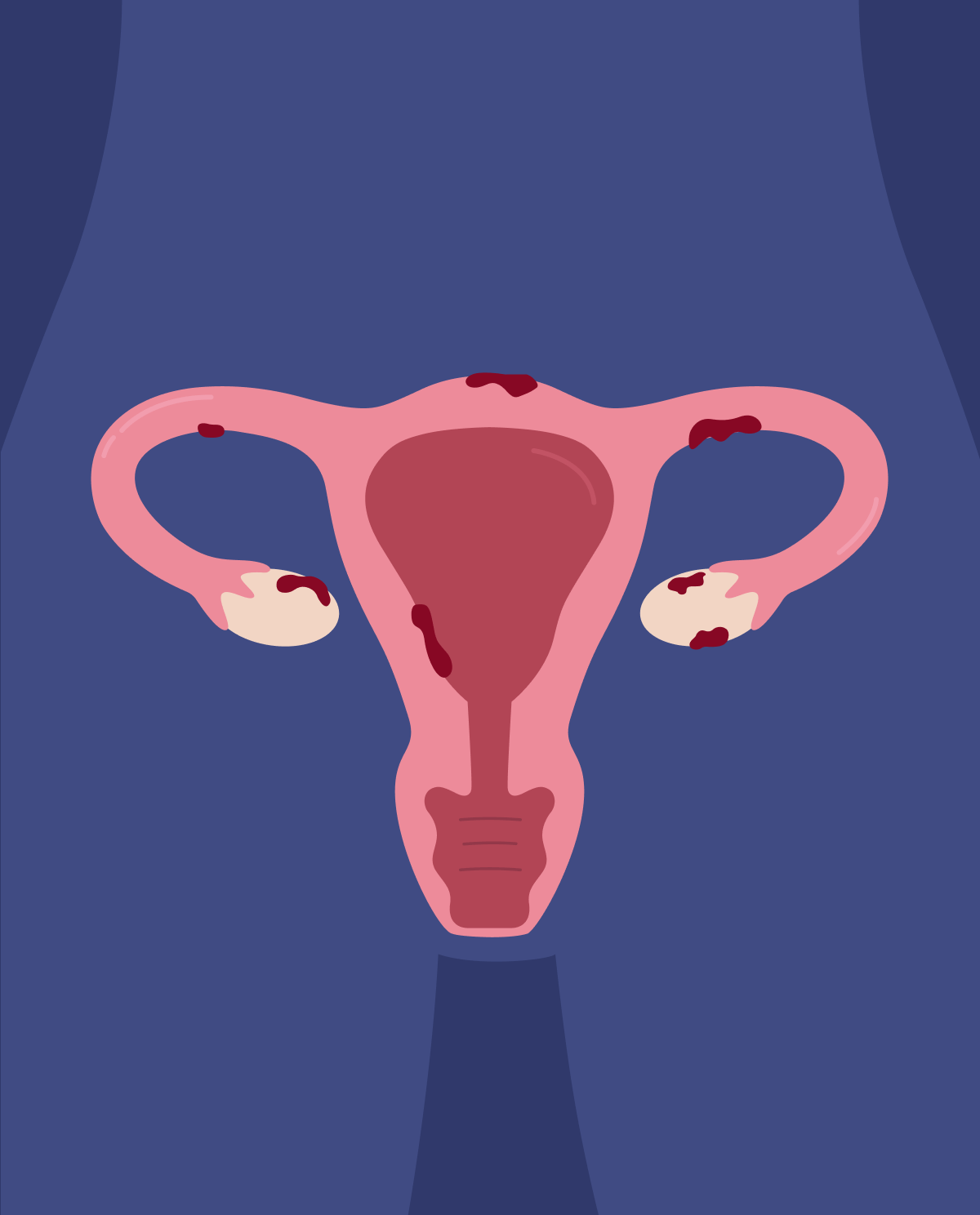
Causes of endometriosis
Although the exact cause of the disorder hasn’t been proven, various possible explanations have been proposed.
- Surgical scarring: during surgery, cells can detach from their normal location and reattach to grow elsewhere. The following can occur after a cesarian section (C-section) or a hysterectomy (procedure to remove the uterus).
- Retrograde menses: instead of flowing out of the body, menstrual blood flows in the wrong direction thus going back to the fallopian tube to enter the pelvic area where it can continue to grow
- Immune disorders: autoimmune activation against endometrial cells growing out of the uterus resulting in inflammation.
- Induction theory: immune and hormonal factors promote the transformation of cells lining the abdomen into endometrial-like cells.
- Lymphatic transport of cells to other areas
Risk factors associated with endometriosis
- early-age menstruation and late menopause,
- nulliparity (never given birth),
- heavy menstruation bleeding lasting longer than 7 days,
- other reproductive tract disorders,
- history of endometriosis in the family,
- period lasting less ho than 27 days,
- low BMI (body mass index).
Symptoms
- very heavy menses or bleeding between periods,
- pain during or after intercourse,
- dysmenorrhea (severe cramping during the menstrual period. It can occur several days before it begins),
- painful urination/defecation during menstruation,
- infertility,
- other nonspecific symptoms associated: bloating, nausea, fatigue, and diarrhea.
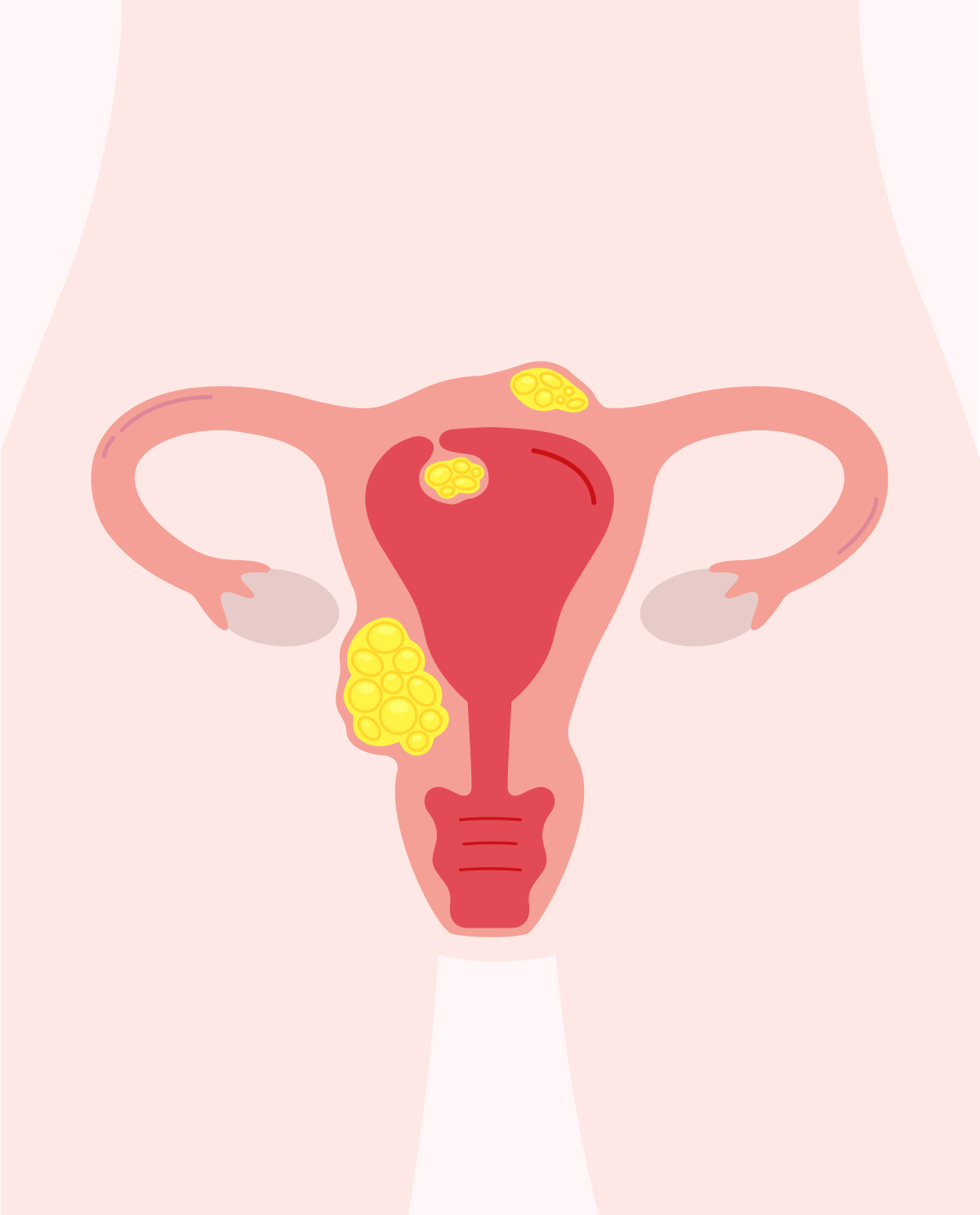
Complications
The most widely reported complication associated with endometriosis is infertility with a prevalence of 30-50% of affected women. Women suffering from a mild to moderate disease may carry a child to term, but it is advised by gynecologists to not delay pregnancy if it is in their plans as the damage to the reproductive system can worsen with time. Endometriosis impedes fertility by preventing the unity of the sperm and egg or by damaging them. Some studies have shown that endometriosis increases the likelihood of developing certain types of cancers such as endometrial-associated adenocarcinoma or ovarian cancer.
Diagnosis of endometriosis
- Pelvic examination: during this physical exam, your gynecologist will manually palpate your pelvic area to search for scarring, cysts, or any other abnormality.
- Ultrasonography (USG): This is performed either via transvaginal ultrasound or by using a transducer placed on the abdomen. It should be of note that a USG won’t give a definite diagnosis of endometriosis, but it would point to clues that could lead to a diagnosis such as endometriomas (cysts that occur in the course of endometriosis).
- Magnetic resonance imaging (also known as MRI): will give the physician a detailed image of the organs to determine the size and localization of the endometriosis.
- Laparoscopic examination: This procedure is done under general anesthesia; the physician will have an internal view of your abdomen. Although more invasive, it gives more information on the extent of endometrial tissue deposits.
Treatment of endometriosis
Treatment mostly depends upon the severity of the symptoms. Endometriosis is usually treated either surgically or with pain medication.
- Pain medication: the following involve non-steroidal anti-inflammatory drugs such as ibuprofen
-
Hormonal treatments are used to slow disease progression. They include:
- contraceptive medications,
- progestin therapy (intrauterine device or implants),
- medication to lower estrogen (aromatase inhibitors, gonadotropin-releasing hormone modulators).
-
Surgery is usually kept until symptoms become unbearable or if the patient would want to get pregnant. During this procedure, the physician will remove the endometriosis patches present but this treatment isn’t a cure, as it can grow back.