Types
- Acute: very common among all age groups, it typically lasts from a few hours to several days. This presents the most common type,
- Persistent: more than two weeks but less than four weeks,
- Chronic: this type lasts longer than four weeks. Symptoms may come and go or be continual during the period.
Causes
Acute and persistent diarrhea
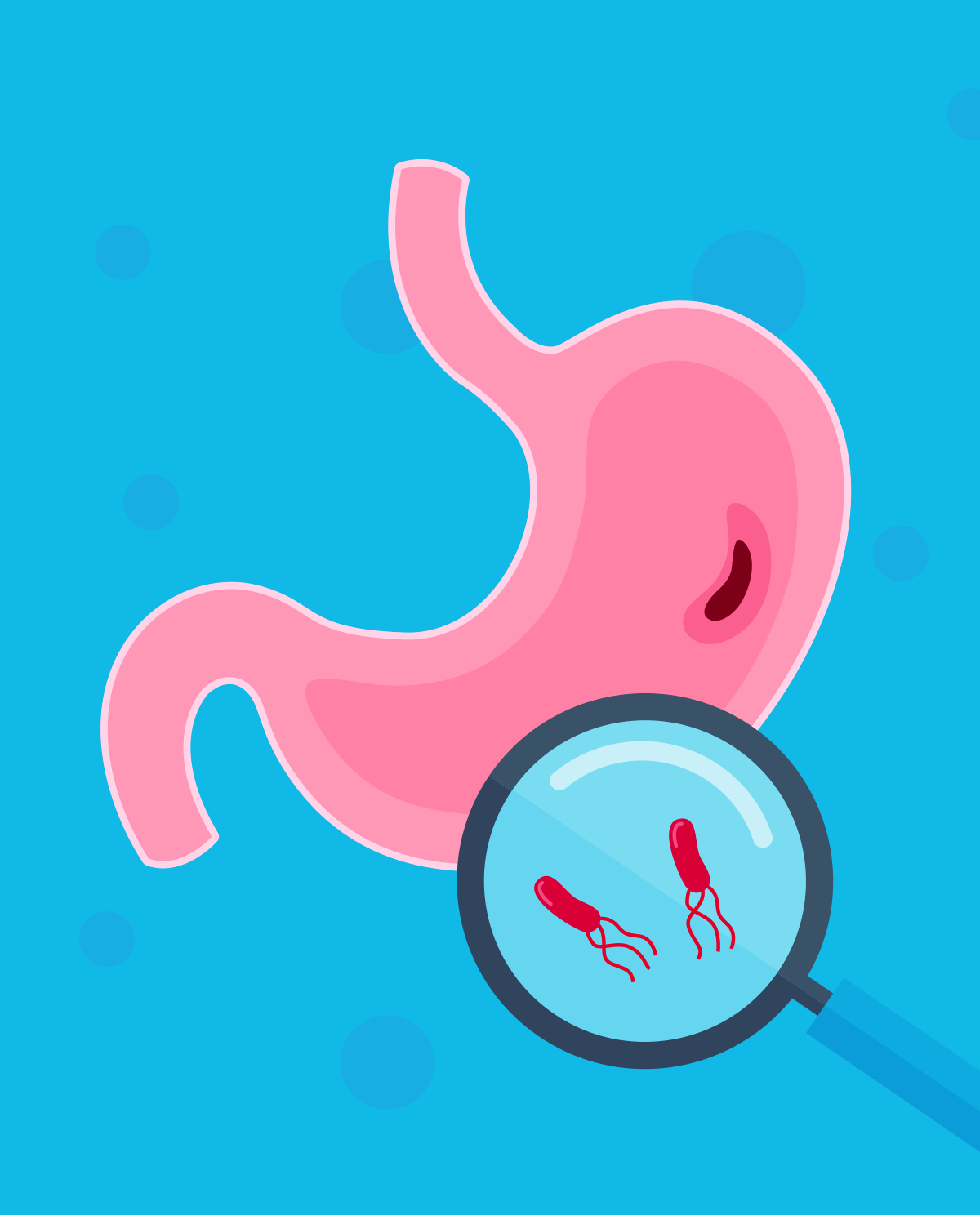
- Infections: three types of infections result in diarrhea. They include viruses (rotavirus and norovirus); bacteria (E. coli, Campylobacter, Salmonella, and Shigella, etc.), and parasites (Entamoeba histolytica, Giardia lamblia, etc.),
- Travelers' diarrhea: this type of diarrhea is usually acute in nature and results from drinking water or ingesting food contaminated with viruses, bacteria, or parasites,
- Medication: various antacids which contain magnesium, antibiotics, and chemotherapeutic drugs have been shown to induce diarrhea.
Chronic diarrhea
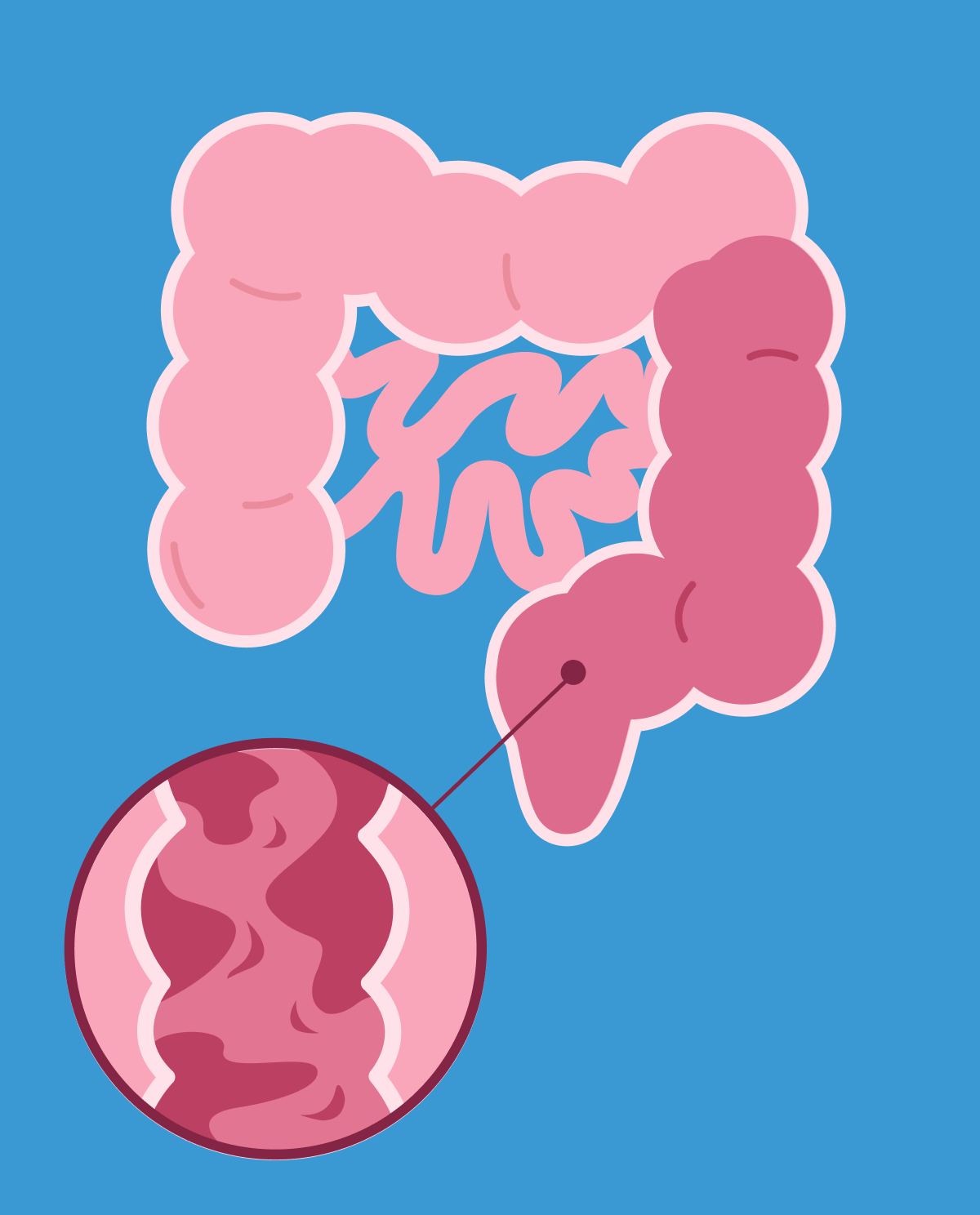
- digestive tract illnesses (Ulcerative colitis, Celiac disease, Crohn’s),
- food allergies (cow or soy milk, dairy, and seafood),
- food intolerance (lactose),
- sugar alcohol consumption (mannitol, sorbitol) may cause bloating and diarrhea,
- abdominal surgeries (gastric, spleen, pancreas, liver, etc.),
- long-term use of antibiotics disrupts the normal gut flora resulting in the overgrowth of unwanted bacteria.
Symptoms
- the urgency of bowel movements and loss of control,
- abdominal cramping,
- abdominal pain,
- nausea and vomiting.
Complications associated with symptoms
- dehydration due to loss of electrolytes and water resulting in lightheadedness, fainting, dry mouth, dark urine (low urine output), thirst,
- malabsorption of nutrients due to rapid passage of stool. The following causes bloating, flatulence (passing gas), abdominal pain, cramping, and foul-smelling stool.
Diagnosis
The doctor will not typically need to find the cause of acute diarrhea as most resolve after a few days. If you present to your GP’s office with bloody stool or fever, then they would need to determine the cause. The doctor will focus mainly on family and medical history in order to elicit a possible diagnosis. In addition to a physical exam, questions asked by your physician about your symptoms would usually cover the following:
- your diet,
- medication,
- the number of stool passages, stool consistency, smell,
- how often it occurs,
- recent travels,
- contact with a sick individual,
- any direct family member with a history of chronic gastrointestinal issues (Celiac disease, Crohn’s, Ulcerative colitis, etc.).
In the case of infection and long-lasting diarrhea, stool samples are collected in order to look for blood or microorganisms. If the patient has had diarrhea and blood for a long time despite any form of prescribed treatment or the family history points to an autoimmune condition, the doctor might ask for a more invasive procedure called colonoscopy.
Treatment
- acute diarrhea is usually treated at home with over-the-counter medication such as loperamide and hydration. (Medical professionals usually do not recommend self-treatment in the case of any systematic signs of infection (fever) or bloody/mucus-tinged stools. It is recommended to see a doctor if diarrhea lasts more than two days or if any signs of diarrhea complications occur,
- in the case of chronic and persistent diarrhea, antibiotic/antiparasitic drugs may be prescribed if a bacterial or parasitic infection is suspected, corticosteroids and other immune inhibiting drugs in the case of Crohn’s, ulcerative colitis.